The Centers for Medicare and Medicaid Services (CMS) published the proposed rule for the fiscal year (FY) 2023 Inpatient Psychiatric Facilities Prospective Payment System (IPF PPS) in the Federal Register on April 4, 2022. This rule impacts freestanding psychiatric hospitals and excluded psychiatric units.
The proposed rule would update rates as well as establish a permanent cap to smooth the impact of year-to-year changes in IPF payments related to decreases in the IPF wage index. Additionally, the rule solicits comments on the results of data analysis of the IPF payment system adjustments and requests information on Measuring Equity and Healthcare Quality Disparities Across CMS Quality Programs.
If finalized, the proposed rate and regulation changes become effective for discharges occurring on or after October 1, 2022. An overview of the proposed rule follows.
Proposed Changes to IPF Payments
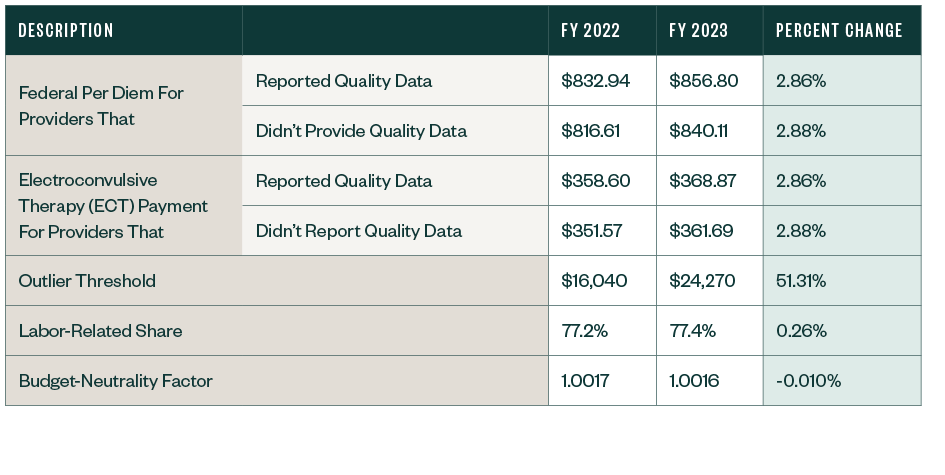
CMS proposed the following updates to the prospective payment rates, outlier threshold, and wage index for the IPF PPS.
IPF PPS Rates
Other Notable Updates
Wage Index Cap
CMS proposed to make permanent its FY 2021 temporary policy of limiting year-over-year wage index decreases to 5%. As such, the FY 2023 wage index won’t be less than 95% of its final wage index for FY 2022. For subsequent years, a provider’s wage index won’t be less than 95% of its prior year wage index.
Inpatient Psychiatric Facilities Quality Reporting (IPFQR)
CMS isn’t proposing any changes to the IPFQR program but seeks comment on items to consider as it works to advance the use of various tools and measures to address health care disparities and advance equity.
Specifically, CMS seeks feedback in five specific areas:
- Identification of goals and approaches for measuring health care disparities and using measure stratification across CMS quality programs
- Guiding principles for selecting and prioritizing measures for disparity reporting across CMS quality programs
- Principles for social risk factor and demographic data selection and use
- Identification of meaningful performance differences
- Guiding principles for reporting disparity results
Economic Impact
The overall economic impact of the proposed FY 2023 changes results in an estimated increase in payments of 1.5% that equates to a $50 million increase in payments from FY 2022.
Public Comments
Public comments can be submitted through 5:00 p.m. EST on May 31, 2022. When commenting, reference CMS-1769-P. Refer to the proposed rule for different ways to submit your comments.
We’re Here to Help
For more information about the proposed rule and potential implications for your organization, contact your Moss Adams professional.
You can also find more insights on our Provider Reimbursement Enterprise Services page.